Artificial intelligence in primary care: a primer
It was exciting to collaborate on this post with Dr. Paulius Mui, a primary care physician and digital health enthusiast. Check out his substack: https://xprimarycare.substack.com
Artificial intelligence (AI) is associated with significant hype, and the phrase is commonplace in the business plans and project proposals of both startups and long-established corporations. Through critical thinking and discussion, we can understand the actual, real-world impacts that these technologies bring to healthcare delivery. In this blog post, we will explain the basic technologies, describe their roles in primary care, and call for primary care physicians (PCPs) to embrace and contribute towards the development of these technologies in the healthcare space.
AI, ML, ANN, and DL are industry buzzwords that are seldom understood yet have become ubiquitous. Source: marketoonist.com
What do artificial intelligence (AI), machine learning (ML), artificial neural networks (ANNs), and deep learning (DL) actually mean?
To kick-off our discussion, we provide very high-level explanations of these terms. This serves to provide readers with a foundation to understand these buzzwords when they appear in promotional materials, news articles, and published research.
Artificial Intelligence
AI is the broadest term used to describe digital processes that mimic human intelligence. In other words, it is not a single technology, but rather an umbrella term that refers to a collection of computer science, statistics, and data analysis techniques that allow computers to draw complex conclusions from data.
There are two distinct types of AI, and understanding the difference between these is a critical first step towards an informed discussion:
Artificial narrow intelligence (i.e., “weak AI” that is restricted to a single task).
Artificial general intelligence (i.e., “strong AI” that can match human intelligence or even demonstrate super intelligence, without being constrained to one particular task).
Only artificial narrow intelligence exists currently. These “weak AI” systems can only perform very specific tasks (such as playing chess) and are wholly incapable of acting intelligently in any use-case for which they are not explicitly designed. The other types of AI (i.e., “strong AI”) are – at this time – found only in fiction.
Artificial general intelligence, which exists only in fiction, would easily bypass even the most sophisticated AI detection systems. Source: https://me.me/
Machine Learning
ML is a type of artificial narrow intelligence. Two types of ML will be explained here:
Supervised ML uses labeled input data (i.e., with known output results) to calibrate and create mathematical input-output relationships. For example, if you want to train a supervised ML algorithm to detect the presence or absence of diabetic retinopathy in retinal photographs, these steps must be followed:
Collect many different retinal photographs.
Get an expert to label each photograph as “retinopathy present” or “retinopathy absent.”
Use some of these labeled photographs to train (i.e., calibrate) the mathematical formulas that make-up the algorithm. This involves adjusting the weighting of the selected input features or variables until the output matches (or approximates) the pre-labeled results.
Test the trained algorithm on the remaining labeled photographs (i.e., those that were not used for training) to ensure that it performs suitably for real-world deployment, when analyzing unseen data.
When the output of a supervised ML algorithm is a discrete or binary result (such as in the above example), the algorithm is solving a classification problem. When the output is a continuous numerical value, the algorithm is solving a regression problem. Note that regression and classification techniques are not new technologies, they have been used by statisticians and data analysts for a very long time. Nevertheless, these techniques form the basis of supervised machine learning algorithms and are classified as artificial intelligence when used by a computer to make decisions based on input variables.
Unsupervised ML algorithms explore unlabeled data to discover underlying patterns, associations, and groupings (aka clusters), without human intervention and without a known output or result. For example, clustering techniques (likely the most common type of unsupervised ML algorithms) can be applied to a large volume of gene expression data to identify multiple, previously unknown, subtypes of a disease (provided that an underlying genetic basis/predisposition exists).
Artificial neural networks and deep learning
ANNs are a type of ML algorithm (either supervised or unsupervised) that is inspired by neurophysiology. In the brain, firing neurons produce a propagation of action potentials, which in turn causes the firing of more neurons, etc. Artificial neural networks mimic this process.
Inputs are combined at nodes (or neurons) at the input layer of the ANN. Similarly, the output of the algorithm is represented by a layer of nodes (or neurons). In-between the input and output layers are the “hidden layers,” each comprising some number of nodes (or neurons). The strength of the connections between the nodes of each layer (among other things) can be adjusted, which allows for very precise tuning of the ANN. In the case of ANNs based on supervised ML techniques, training the ANN involves adjusting these connection strengths, effectively changing the structure of the network to produce a desired output using labeled input data.
An input signal (comprising the input variables) will propagate from the input layer, through the hidden layer(s) and reach the output layer. A DL algorithm is simply an ANN with more than one hidden layer of nodes.
Architecture of an ANN system, including the input, hidden, and output layers. Source: ibm.com
In summary, AI is an umbrella term that encompasses multiple techniques used by computers to draw complex conclusions from data. ML is a type of AI, ANNs are a type of ML, and DL is an ANN with more than three layers of nodes. Statistics form the building blocks of each of these technologies.
The relationships between different subtypes of AI.
AI and healthcare
There are many examples of AI products and services in healthcare, some of which have already received FDA approvals for clinical use. AI solutions are available for virtually every physiological system, as shown in the table below. For a deeper dive, explore Dr. Bertalan Mesko’s database of FDA approved AI algorithms.
|
System |
Example(s) |
|
Otorhinolaryngology |
Harnessing the Power of Artificial Intelligence in Otolaryngology and the Communication Sciences |
|
Ophthalmology |
|
|
Cardiology |
|
|
Pulmonology |
|
|
Gastroenterology |
|
|
Dermatology |
|
|
Orthopedics |
|
|
Nephrology |
|
|
Infectious disease |
|
|
Urology |
|
|
Gynecology & Obstetrics |
Artificial Intelligence: A New Paradigm in Obstetrics and Gynecology Research and Clinical Practice |
|
Hematology |
How artificial intelligence might disrupt diagnostics in hematology in the near future |
|
Rheumatology |
Use of artificial intelligence in imaging in rheumatology – current status and future perspectives |
|
Endocrinology |
Machine Learning Applications in Endocrinology and Metabolism Research: An Overview |
|
Oncology |
|
|
Neurology |
|
|
Psychiatry |
|
|
Allergy and immunology |
Artificial intelligence in the diagnosis of pediatric allergic diseases |
|
Radiology |
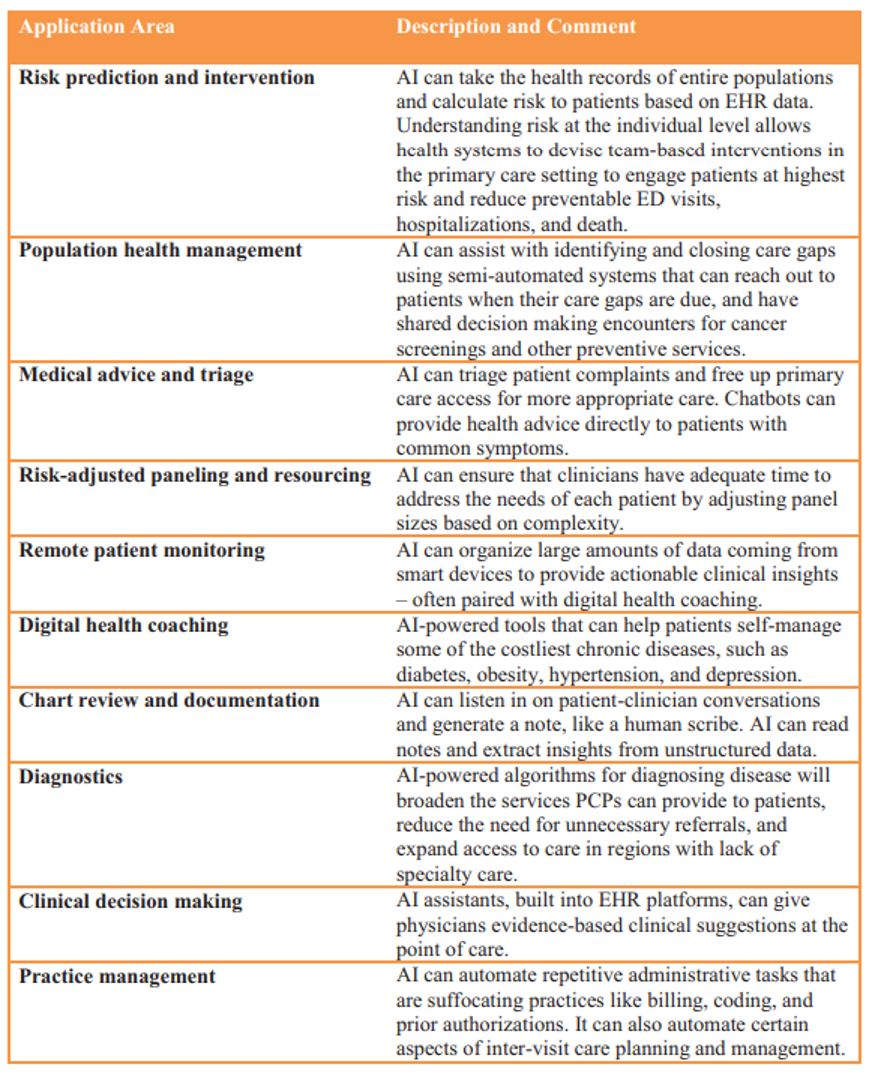
Dr. Steven Lin has written extensively about ways AI can impact the work of clinicians. In his recent paper, he brilliantly outlines ten areas across healthcare in which AI is playing a transformative role.
We will focus on the primary care setting for the remainder of our discussion, because this is the medical specialty where the potential impact of AI is greatest. This opinion is championed by Dr. Lin. who has called for a national strategy to implement AI/ML in primary care.
AI in the primary care setting
It’s no surprise that more than half of all patient visits in the US are in primary care. PCPs are the first port of call for most patients’ physical and mental health needs, spanning a multitude of contexts including acute, chronic and preventive services. Because PCPs navigate clinical, behavioral, and social data across a vast number of diagnoses and disciplines, they “can add value to practically any AI use case in health care.” Each of the core functions of primary care (aka the 4 C’s: first contact, comprehensiveness, care coordination, and continuity) demonstrates a mutually beneficial opportunity for collaboration between PCPs and AI developers.
There is strong evidence to support the formation of centers of excellence, in which PCPs with special interests provide comprehensive care and coordinated management for patients with multiple chronic conditions (e.g., diabetes, heart failure, kidney disease, COPD, etc.). Higher patient volumes coupled with more complex disease states and worsening administrative burden necessitates technological interventions. We have extracted and expanded upon Dr. Lin’s ten groups (which are applicable to all healthcare settings) to identify five distinct roles of AI, which will routinely assist PCPs in everyday practice:
AI to triage patients and identify who needs to see the PCP and how urgently
Most PCPs acknowledge that workloads in their practices are steadily increasing. This anecdotal evidence is strongly supported by real world data, which also shows that we are approaching a saturation point. AI will be implemented to triage acute patients before they present to their PCPs. Chatbots and online questionnaires will engage with patients and use inbuilt AI to rank the importance of presenting complaints. These systems are trained to identify “red flags” and respond accordingly, including immediate referral to an emergency room if appropriate. Less urgent consultations can be scheduled automatically for off-peak times. Events that can be handled by physician assistants or allied healthcare providers can be automatically redirected. This ensures that emergency cases are consistently prioritized, and will stabilize PCP workloads and decrease waiting room usage (and the dissatisfaction and anxiety that accompanies it).
Preventative medicine and screening
Routine screening for a plethora of pathologies is becoming common practice, and numbers of patients in primary care who are considered “high risk” for these pathologies are growing. Historically, many screening examinations have not been possible without referring to specialists. AI effectively brings specialist skills into the primary care setting and can be employed routinely for eligible patients. Increased accessibility, affordability, and convenience has been shown to increase uptake of screening services by patients. For example, AI software and an automated fundus camera in a PCP’s practice can screen all patients with diabetes before retinopathy symptoms emerge, and indicate which patients require escalation of care.
Diagnostic aid
In contrast to the previous use-case (routine deployment of AI for screening), AI will also be used by PCPs on an ad-hoc basis for diagnostic support. For example, AI-powered assessments will support PCPs who are presented with an abnormal skin lesion, and will provide consistent recommendations 24/7 and without tiring.
To supplement this section, modern technologies underpinned by AI (smart wearables, CGMs, etc) will also direct patients to their PCPs when abnormal measurements are detected, and patients will arrive with quantitative data and AI-suggested diagnoses. It will remain the responsibility of the PCP to confirm the diagnosis or refer the patient.
Support PCPs by providing targeted, up-to-date medical information
AI systems are being developed to collect and organize important information from a patient’s entire history. This data and the current clinical findings can be combined with the very latest published research and clinical guidelines to ensure that treatments and protocols are always up-to-date and the patient’s individual background is taken into account. Relevant drug dosages, interactions, and contraindications will be presented to PCPs before they prescribe, and geographic factors (e.g. local patterns of antimicrobial resistance, stock availability, etc) can be accommodated.
Provide administrative support
Most physicians are currently overwhelmed by computer/paperwork, and general administrative tasks. The primary care environment is no exception, and patients frequently complain that their PCP “barely even looks at them anymore” or “hardly looks up from her computer.” In many cases, this behavior is eroding the doctor-patient relationship, which is especially critical in the primary care environment.
New AI-powered solutions exist that act as physician assistants, using connected clinical devices (e.g., intelligent blood pressure cuffs) and voice recognition to automatically record consultation details. These solutions may restore humanity to primary care and allow PCPs to focus more on patient engagement without compromising their documentation and medicolegal responsibilities.
Does AI pose a professional threat, or is it an asset for PCPs?
We have emphasized the distinction between real-world “artificial narrow intelligence” and fictional “artificial general intelligence.” This distinction is important because AI fear-mongering within the medical profession is frequently based upon unrealistic perceptions about the current state of AI technologies (perhaps from artificial general intelligence shown in television and movies).
Artificial intelligence is being utilized in medicine to support (i.e., not replace) human physicians, and it is likely that the primary care environment is where these technologies can have the greatest impact. AI will improve practice efficiency through advanced triage, delay disease progression through automated screening, supplement practices with specialist-level knowledge for diagnostic support, feed tailored and up-to-date information to providers, and boost the doctor-patient relationship by allowing PCPs to truly engage with their patients. However, no artificial narrow intelligence can replace a PCP’s emotional intelligence, empathy, and ability to coordinate and deliver a truly holistic healthcare experience to patients.
Ethics and responsibilities of the primary care profession for AI deployment
It is essential that PCPs help to mold the development of AI systems in healthcare. It is inevitable that these technologies will penetrate the healthcare space, and resistance to this is both counterproductive and unrealistic (analogous to an airline pilot refusing to use an autopilot system). Acceptance of new, clinically proven technologies demonstrate a doctor’s commitment to remain up-to-date and to use evidence-based medicine to enhance patient care.
At the same time, we recognize that it’s important to remain vigilant about potential pitfalls and biases that this technology bears. Without guidance from PCPs, AI might grow into a system plagued by endless digital prompts, confusing and irrelevant diagnoses, mass adoption of defensive medicine, and undue patient stress arising from poorly communicated over/under diagnoses. As the frontline for the medical profession, PCPs can scrutinize the impact of AI systems in healthcare, and provide invaluable insights and feedback for developers. The primary care environment is also where most doctor-collected data is recorded (both measured clinical data and the biopsychosocial determinants of health).
There is an abundance of literature available that describes the ethical considerations and the various biases relevant to AI-powered healthcare technologies, so we only briefly cover these important topics here. In our earlier explanations of AI and its subtypes, we discussed the importance of training data for AI development. Biases that exist within the training dataset will almost certainly manifest in the final algorithm(s), and these biases would translate to healthcare inequality and unfairness. AI developers must aim to eradicate these biases from the very start of the development pipeline, including data collection/sampling, modeling, and labeling. Physicians and AI developers must collaborate, with each providing expertise to avoid potential discrimination (e.g. skin lesion classification by AI, that works inconsistently in certain ethnic groups due to an insufficiently diverse training dataset). Both clinical and data expertise must be represented in teams that develop, review or approve AI systems for healthcare applications.
If any inconsistencies do appear in the approved version of an AI-powered healthcare product, it is very likely to be noticed first by the PCPs. It is the responsibility of PCPs to embrace vetted AI technologies to ensure that they are offering the latest knowledge and healthcare tools to their patients. PCP participation also ensures that this technology is molded and developed in a way that boosts healthcare accessibility and quality, as well as keeps it accountable and equitable.